Abstract
Allogeneic hematopoietic cell transplantation (AlloHCT) is the only curative approach for myelofibrosis (MF). However the significant risk of morbidity and mortality associated with this treatment necessitate careful patient selection and intense peri-transplant management. Here we report on the clinical outcome of a large cohort of MF patients who underwent alloHCT with fludarabine/melphalan (FluMel) condition regimen at City of Hope (COH).
A total of 110 consecutive patients with MF (primary MF: n=58, secondary MF: n=52) without prior acute leukemic transformation, underwent allo-HCT between 2004 and 2017 at COH. Median age at the time of transplant was 58.5 years (range: 38-72 years) with median interval from diagnosis of primary or secondary MF to HCT of 15.2 months (range: 1.6-332.5 months). A majority of patients (n=107) received peripheral blood stem cells and 3 were transplanted with bone marrow as stem cell source. AlloHCT donors were matched related (MRD: n=49), matched unrelated (MUD: n=32), mismatched unrelated (MMUD: n=27), mismatched relative (n=1), or haploidentical family (n=1). Dynamic international prognostic scoring system (DIPSS) score at the time of alloHCT was Intermediate-2 or high risk in 83 patients (76%). All patients received FluMel conditioning. Graft-versus-host disease (GVHD) prophylaxis was predominantly sirolimus/tacrolimus-based regimen, n=100 (91%). Of the 110 patients, 16 had splenectomy prior to alloHCT. Cytogenetics information was available for 104 out of 110 patients; among which, 60 patients had abnormal cytogenetics including but not limited to deletion 20q, trisomy 8 and trisomy 9.
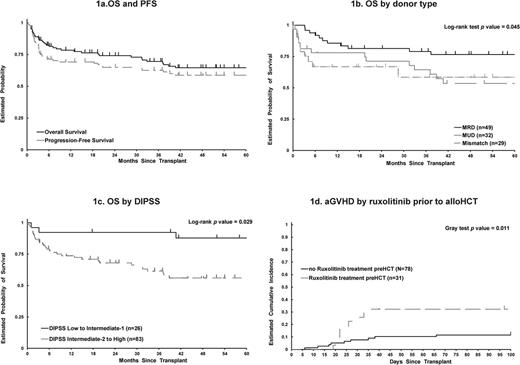
All but 2 patients were engrafted. After median follow-up of 56.8 months (range: 1.3-158.5 months) in surviving patients, 2- and 5-years overall survival (OS) were 74% (95% CI: 65-82%) and 65% (95% CI:54-73%), respectively (figure 1a.); 100 days, 2- and 5-years non-relapse mortality (NRM) were 12% (95%CI: 0.06-0.18), 18% (95% CI: 11-26%) and 24% (95% CI: 16-33%) (figure 1b.); 2- and 5-years. cumulative incidence of relapse (CIR) were 17% at both time-points (95% CI: 11-25%). In univariate analysis MMD and MUD were significantly associated with worse OS compared with MRD (HR: 2.60 [95% CI6: 1.15-5.88] and HR: 1.99 [95% CI: 0.94-4.18], P value= 0.045, respectively) (figure 1c.), in consistency with increased in NRM in these groups (HR: 3.24 [95% CI: 1.31- 8.03), for MMD and 2.48 [95% CI: 1.02-6.04], for MUD, P value=0.029). Lower DIPSS score at the time of transplant was associated with better OS, compared to intermediate-2/high risk (HR: 0.39, 95%CI: 0.16-0.94, p=0.029). Interestingly splenectomy prior the transplant was associated with higher relapse risk (RR), RR= 3.21 (95% CI: 1.24-8.33) (P value=0.018). Cytogenetics abnormalities were not associated with transplant relapse or other outcomes in our cohort. Mutational changes are being tested in pre-transplant samples and will be reported later.
Incidence of grade II-IV and III-IV acute GVHD at 100 days were 45% (95% CI: 36-54%) and 17% (95% CI: 11-25%), respectively. At 36 months, cumulative incidence of all chronic GVHD was 66% (95% CI: 55-74%) and extensive chronic GVHD was 59% (95% CI: 49-68%). In this cohort, 32 patients that were treated with ruxolitinib prior to allo-HCT had higher risk of grade III-IV acute GVHD (p=0.011, RR 3.15 [95% CI: 1.31-7.58]) (figure 1d.). Furthermore, ABO incompatibility was associated with higher risk of acute GVHD grade III-IV (p=0.004, RR 4.09 [1.50-11.12]).
In summary, we are presenting one of the largest single center experiences of FluMel-based allo-HCT for patients with MF. We showed that this patients have an excellent OS (64% at 5 years) with low risk of relapse (17% at 5 yrs). The risk of NRM was acceptable considering the relatively older age of a large subset of patients (43 aged >60yrs at alloHCT). Interestingly, prior use of ruxolitinib increased the risk of grade III-IV acute GVHD, possibly due to known inflammatory cytokine rebound. Extended use of ruxolitinib until day +30 is currently being evaluated in a prospective trial (NCT02917096).
Pillai: Trillium Therapeutics: Research Funding. Salhotra: Kadmon: Consultancy. Stein: Stemline: Consultancy; Amgen: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.